- News and Stories
- Blog post
- Safety Net
Working with the Data You Already Have to Improve Benefits Delivery

Since 2022, Code for America has been working with state health care agencies to improve outcomes for ex parte renewal, an automated process that uses already-existing data to determine someone’s eligibility for continued health care coverage. That already-existing data can come from state-administered program data, like the Supplemental Nutrition Assistance Program (SNAP) or Temporary Assistance for Needy Families (TANF), or external data sources such as the Social Security Administration or the Internal Revenue Service. Utilizing this process significantly reduces administrative burdens for beneficiaries, who no longer have to complete a renewal form, and state administrators, who no longer have to review and process renewals. It’s a rare win-win in the public health benefits delivery space.
Improving ex parte outcomes became especially critical following the conclusion of the COVID-19 Public Health Emergency (PHE), commonly referred to as “the unwinding.” During this period, the Centers for Medicare and Medicaid Services (CMS) required all states to renew a record 93 million Medicaid and Children’s Health Insurance Program (CHIP) beneficiaries within a one-year timeframe. Many states recognized the efficiency of ex parte renewal and put resources into enhancing this process to address the surge.
But some states are deeply hesitant to make changes to their systems due to a lack of data maturity. Our experience has shown that this doesn’t have to be a barrier to investigating and enhancing systems. Regardless of a state’s capabilities or access to specific data, it is possible to successfully do this work and make meaningful improvements.
What exactly is data maturity?
Data maturity is a measure that reflects an organization’s ability to effectively collect and leverage data to inform decision-making. In the context of ex parte renewal, high data maturity means having a clear understanding of why and how many beneficiaries are falling out of the ex parte process. Having low data maturity, on the other hand, might only provide an overview, like whether or not someone passed the ex parte process, without understanding the specific reasons or points at which they fall out. This lack of detail can make it difficult to determine where to begin making improvements.
How data maturity affects a state’s ability to enact change
In high data maturity states, when figuring out how to improve ex parte outcomes, you may look at all the automatic decision outcomes the system makes to see exactly why beneficiaries fail ex parte. With this specific outcome data, you can rapidly uncover mismatched policies or overly restrictive system implementation.
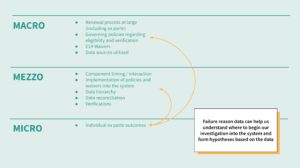
Things look different in low data maturity states. This is our strategy for improving ex parte outcomes in those situations:
-
- Gather all existing implementation best practices, policies, assessment tools, and administrative guidance from federal entities. Based on these resources, we outline how a system should operate during ex parte renewal, as well as questions we could ask state staff and technical vendors to uncover current system behavior.
- Map out the end-to-end ex parte and standard renewal process with state stakeholders and technical vendors. We look at things like how and when the system makes data interface calls, how the system reconciles income information between data sources, and the process of flagging income and resource-based verifications.
- Develop hypotheses based on what we uncover from the mapping process, and work with a state’s technical vendor to confirm or reject those hypotheses. We develop system implementation questions that enable us to dig deeper in system behavior. We ask for specific data to try to confirm or reject hypotheses and generate opportunities for improvement.
- Visualize the opportunity to quickly align on priorities. By creating visualizations that simplify systems and highlight best practices, we can involve less technically experienced state administrators in the discussion, aligning everyone on important areas for system improvement.
This work in action: Learning from Colorado
When we partnered with Colorado to improve their ex parte renewal process, we struggled to collect detailed failure data, and so developed an approach to examine different levels of focus within the system. Here are two examples of how that worked:
We ensured reasonable compatibility was not applied at ex parte to make an eligibility determination. Reasonable compatibility is a Medicaid policy used to determine if a beneficiary’s self-reported income matches their electronically verified income. This is especially useful during the application process or standard renewals when new self-reported information is provided. However, during an ex parte process—when external data is first used to make a decision—it isn’t appropriate to compare that data with case information that’s a year old.
But still, many states continue to apply reasonable compatibility during ex parte—and our findings revealed that Colorado was using outdated case file data when applying reasonable compatibility. If a beneficiary didn’t meet the criteria, they were issued an income discrepancy letter requesting additional verification.
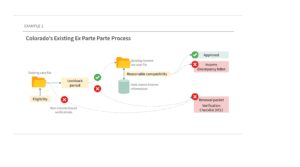
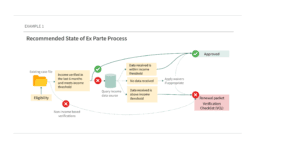
Based on CMS guidance and Center on Budget and Policy Priorities best practices, we recommended that Colorado remove reasonable compatibility from their process and directly use electronically verified income. This change meant that anyone who met the income criteria would pass ex parte, and those above the income limit would receive a renewal packet. When CMS later clarified its stance that reasonable compatibility does not apply during an ex parte renewal, Colorado was ahead of the curve.
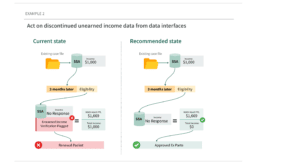
We suggested that the system shouldn’t flag a verification for an income source that has been shown discontinued from a reliable data source. When digging into system functionality with Colorado’s technical vendor, we learned that if an individual stopped receiving income from a reliable source, they were still asked for verification. This means that when someone loses an unearned income amount, the system removes them from the ex parte process instead of running eligibility without that income source. In recent guidance, CMS stated that “no information returned” can support a determination that the beneficiary does not have that specific type of income anymore. This logic can be applied to any other unearned income that can be verified using automated interfaces.
Following our best practices review, we identified 11 actionable opportunities to improve Colorado’s ex parte process. Colorado has already addressed a bug we found in their implementation of a common unwinding waiver, which we estimate will help about 4,600 clients each month. If Colorado acts on all of our recommendations, we estimate about 11,975 clients each month will be ex parte approved, an increase of 16%.
Expanding this work in other states
Colorado is not alone in facing the challenges we’ve outlined. State administrations often lack the bandwidth or tools to ensure their systems deliver as expected—yet this should not be a barrier to progress. Now that many of the CMS unwinding waivers and flexibilities are permanent, states that were previously hesitant to adopt these options due to uncertainty about their future should reconsider—and states that took advantage of these are ahead of the curve.
To be successful in this work, states must dig into the heart of how their systems translate policies into system behavior. Even without the data to diagnose system behavior quickly, following best practices from federal sources and other trusted organizations can help generate the right questions, leading to clear answers and the ability to gather supporting evidence. This work is possible; it’s up to states to be proactive to ensure the best possible outcomes for all.