- News and Stories
- Blog post
- Safety Net
Cell Phones as a Safety Net Lifeline

Eligible people struggle to maintain their case status for critical safety net services, often due to administrative hurdles and poor communication. Code for America piloted text message reminders to support Louisianans, which helped clients avoid costly churn. Text messages are an underrated, efficient solution for human service agencies to meet client expectations and improve case outcomes.
Context: The safety net in Louisiana
Rodney* waited until the clock struck midnight to go get food, even though he was hungry all day. His food assistance card was typically reloaded then, but when he went to the store that night, his card was denied. He tried six more times to buy food that night, but was denied each time. He didn’t know why.
After walking to the local public benefits office the next day, he learned that he had missed submitting a required semiannual paper report to keep his case open. Rodney checks his mail about once a week by walking to the homelessness outreach center, but the paper form didn’t arrive. While pursuing a degree, working part-time, and fulfilling chores at his transitional housing, Rodney was also mourning the recent loss of his sister. The paper-based renewal system didn’t serve his life circumstances—the precise circumstances that were responsible for Rodney needing the support of food assistance.
The social safety net reaches deep into daily life in Louisiana. About half of Louisiana households use safety net services or are one paycheck away from needing them. More than three in four children in Louisiana receive Medicaid benefits.
A common thread in the delivery of safety net programs like SNAP and Medicaid is the extraordinary difficulty eligible clients face in maintaining their benefits. “Churn” happens when clients’ benefits are revoked, but they rejoin the program soon after. Churn often occurs when clients simply do not know what they must do to maintain benefits, or when they struggle to complete the procedural tasks mandated of them.

Frequently, clients only realize that they have lost their benefit when they try to use it—an EBT card is unexpectedly empty at the start of the month, or a provider informs them their health insurance is no longer valid. These moments are accompanied by deep anxiety and financial insecurity. As one client put it, “Every six months, I basically start over.”

Churn is costly to the state of Louisiana as well. It takes significantly more time for a caseworker to process a new application than it does to maintain a current one. Overburdened document processing centers sort the same documents submitted months earlier. Customer service call centers receive panicked or angry calls from clients who need support. In the Integrated Benefits Initiative, we asked ourselves: how would a human-centered safety net manage the challenges of churn?
Developing text message reminders to reduce client churn
Code for America selected Louisiana as one of five partner states for an Integrated Benefits Initiative technology pilot to improve government services. Our initial research and discovery period yielded two important insights. First, for clients, a backdrop of hardship and volatility means stability is the exception, not the norm. Second, clients overwhelmingly prefer electronic communication (as opposed to mail), with most relying solely on their mobile phones.
Phones are people’s lifelines, and yet are absent in most clients’ experience with Louisiana’s safety net services.
Taking these insights together, Code for America and Louisiana developed and trialed LA’MESSAGE, a text message-based reminder service for Medicaid, SNAP, TANF, and WIC clients. The goal was to help clients understand and complete critical processes at case renewal moments, while reducing burden for caseworkers.
“We are committed to making sure Louisianans who are eligible maintain their Medicaid coverage, so we appreciated this opportunity to partner with Code for America, learn more about our recipients’ needs, and innovate with them.”
Clients received the first reminders from LA’MESSAGE in April 2019, beginning with a few dozen WIC New Orleans clients and then rapidly scaling to hundreds of clients in May 2019, thousands by June 2019, and tens of thousands in the following months. By the close of the pilot in December 2019, more than 108,000 Louisianans across four safety net programs were offered reminders, with almost 27,000 opting in to the program.

Using feedback to develop client-centered reminders
Code for America used an iterative, human-centered process to gather feedback from clients and staff to improve the messages and subsequent case outcomes. Before we sent our first message, we gathered feedback from clients on what types of information would be valuable to them, and what language was clear and actionable. We employed a range of user research techniques, including:
- Interactive, in-person interviews, including sorting and prioritization exercises
- Contextual inquiry to observe client actions in their homes and public settings like libraries
- Remote user testing and electronic surveys

During the pilot, direct user feedback informed adjustments to the various LA’MESSAGE reminder campaigns. For instance, while we envisioned and launched LA’MESSAGE deliberately as a one-way reminder service, clients interacted with the messages in unexpected ways. When clients replied to the text messages, we developed an auto-responder to redirect them to existing state customer service channels for their particular safety net program. When clients called the phone number associated with the text messages, we recorded an automatic voice message to do the same.
Throughout the pilot, we used experimental methods to test the impact of new variations on the reminders. In one experiment, we A/B tested two framings for renewal language with approximately 11,000 Medicaid clients: professional and friendly. Clients who received the professional framing returned their renewal packets at a higher rate than those who received the friendly framing (37.6% vs. 33.8% respectively), which led us to use professional framing in future campaigns. Follow-up qualitative research indicates the effect may be related to trust that the sender of the message is the program agency, rather than a fraudulent message.

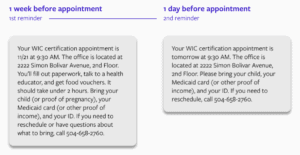
In a second experiment, we tested whether the number of reminders for an upcoming WIC appointment was most successful in helping clients show up to their appointment. Clients who received one, two, or three messages all showed up at similar rates, suggesting that even just one specific reminder can significantly improve outcomes for clients who have recently opted into a reminder campaign. The higher level takeaway is that rigorous testing and iteration can reveal surprising insights into a specific service delivery context. (It’s worth noting that in other settings, Code for America finds that more reminders typically improve outcomes. It may be that in this specific context, the users who opted-in were already the most motivated and able to complete the interview, making additional reminders unnecessary.)
As the clients completed reminder campaigns, we folded in other methods of user feedback. Approximately 1,100 clients received an optional customer satisfaction survey to rate their experience and provide open-ended feedback. The general themes affirmed the value of text messages, while also speaking to the importance of providing accurate, timely information. Alongside this wider survey, Code for America conducted feedback sessions with clients in their homes, providing deep, contextual feedback on the broader experience of trying to maintain benefits.
What did LA’MESSAGE deliver for clients?
LA’MESSAGE delivered timely, specific reminders to clients with eleven case types spanning four distinct safety net programs. We collected data on clients who opted-in compared to a baseline of those who did not opt-in. In every instance, the available data indicates that LA’MESSAGE reminders improved outcomes related to churn, at times dramatically:
- 750+ WIC clients improved their kept appointment rate by 79%, with 52% of clients successfully renewing over the baseline of 29%
- 450+ SNAP Simplified Reporting clients increased their case maintenance rate by 21%, with 81% of clients successfully renewing over the baseline of 67%
- 450+ SNAP Redetermination clients increased their case renewal rate by 37%, with 70% of clients successfully renewing over the baseline of 51%
- 58 FITAP clients increased their case renewals rate by 13%, with 71% of clients renewing over the baseline of 63%
- 9,900+ Medicaid renewal clients increased their annual case approval rate by 67%, with 25% of clients successfully renewing over the baseline of 15%
- 6,200+ Medicaid income check clients increased their verification response rate by 56%, with 25% of clients returning the document over the baseline of 16%
The broader impact is larger than the final numbers suggest. A 2014 study by the Food and Nutrition Service estimated the administrative costs to state agencies associated with churn to be $80 per SNAP client. It’s impossible to quantify the frustration, confusion, and anxiety that clients face when they unexpectedly lose their benefits due to an administrative barrier, but we can conservatively estimate multiple hours saved per client who is able to avoid losing their benefit and beginning a new application entirely. Finally, besides avoiding these human costs of churn, the LA’MESSAGE pilot demonstrated that innovative states can successfully meet clients’ modern communication expectations.
“The goal is to be responsive to the daily realities of the Louisianans we serve and understand how compounding stress can impact how they communicate with us, with the ultimate objective being making sure those who are eligible follow through with important requirements.”
The LA’MESSAGE pilot unambiguously proved that text message reminders are an exceptional solution to persistent challenges in Louisiana:
- Reminders improve outcomes, nearly doubling key metrics in some cases.
- Reminders supplement communication gaps from undelivered paper mail, indecipherable notices, clunky online portals, and overburdened call centers.
- Reminders create feedback loops with real data from real users that can serve as an early warning when the benefits program is not working correctly.
- Reminders reach clients of all backgrounds cheaply and efficiently, costing pennies to send while maintaining extremely high delivery rates.

We are grateful for the leadership and initiative of our partners at the Louisiana’s Department of Children and Family Services, Department of Health, the Office of Technology Services, and the Louisiana Governor’s Office.
For more information on the text message campaigns and underlying design principles, please see our demonstration website. For more information on the LA’MESSAGE pilot or other Integrated Benefits Initiative work, please reach out at integratedbenefits@codeforamerica.org.
For a deeper dive into the details, read the full report.
This work was supported by our generous partners and donors, including the Chan Zuckerberg Initiative and Walmart.org
*This client’s name has been changed to preserve their privacy.